The upstream oil and gas industry has for decades dealt with a talent shortage and its subsequent technology stagnation, termed “the great crew change”. It’s inspired some hard looks at industry practices, and has propelled technology advancements and strategic realignments. The nurse call industry needs an awakening of this sort, that takes us beyond low-level building system and towards… what? With nearly full market penetration, minimal system differentiation, and encroaching competition, nurse call faces the existential question: where do we go from here?
Provider requirements have outgrown traditional nurse call
Compared to the pace of technology in the consumer markets, and in other healthcare applications, traditional nurse call looks like something from a museum of medical history. Some have questioned whether it remains relevant at all. The answer: not in its current form.
The need for immediate, actionable data leaves legacy systems behind. It isn’t enough to turn on a light and play chimes; it isn’t enough to place a glorified phone call to the bed; it isn’t enough to provide limited reporting with only a few data points. IP technology is no longer cutting edge, nor is SIP, ASM, TAP, SNMP, BACNet or any similar technologies commonly deployed alongside nurse call.
Providers need to exchange data across systems. Real interoperability, not just lip service paid at industry conferences. Care delivery models change daily, requiring the integration of more applications, and the ability to change processes on the fly. Existing and new pieces of the healthcare system need to communicate much more effectively than they have hitherto.
Traditional nurse call is too hardware-oriented, too costly, and above all too limited for a provider to invest any more than necessary. If all that’s required is a checked box for regulatory compliance, why not choose the least expensive system that checks the box? Satisfy the physical button and light requirement with commoditized hardware, and address communications and data exchange upstream?
Providers have more options than ever, and a conservative roadmap of incremental updates to the same buttons and lights isn’t going to satisfy them. The future of healthcare communications technology is software, and our roadmap needs to move us away from the outdated association with “call bells”. Nurse call, the term and the concept, is antiquated. The value we add is the data; hardware-based communication barely gets you in the door.
Regulatory certification will not keep competition away
The heavy processes imposed by the regulatory environment often result in a lack of innovation from established companies, leaving us vulnerable to disruption. What displaces traditional nurse call will not be a nurse call startup. It will be a comprehensive software platform that subsumes all the functions of nurse call with minimal loss.
Despite the artificial barriers to entry for hardware manufacturers, more and more software applications offer functions that have traditionally belonged to nurse call. In one platform, providers can get alarm and event notification, workflow, messaging and voice calling, all linked to the EMR and other clinical systems. These platforms offer creative workarounds to nurse call’s limitations. In light of this new breed of communications solution, it doesn’t matter which vendor’s hardware captures the button presses; all the intelligence, and thus all the value, lies in another system.
Disruption may come somewhere upstream. If a hospital can install a $29 smart speaker in every room, backed up to a cloud server housing all their data, with an enterprise analytics application built-in, and an AI engine to predict outcomes, more than just nurse call will be affected. We can’t ignore the possibility that well-funded consumer companies, attempting to make a foray into healthcare, are working to overturn the compliance requirements.
This will all take time. Think of it like a foundation problem on your home. At first, all you notice are a few cracks at the joints, doors that don’t close. But over time those problems compound, and if not corrected, your house will collapse in slow motion. Traditional nurse call will not evaporate overnight, but more and more critical functionality will reside in other applications, leaving nurse call’s purview back where it began with physical buttons, lights, and other low-end hardware. In its current form, nurse call is relegated to the lowest rung on the communications ladder: generating events without context.
The Solution: A Real Time Health System
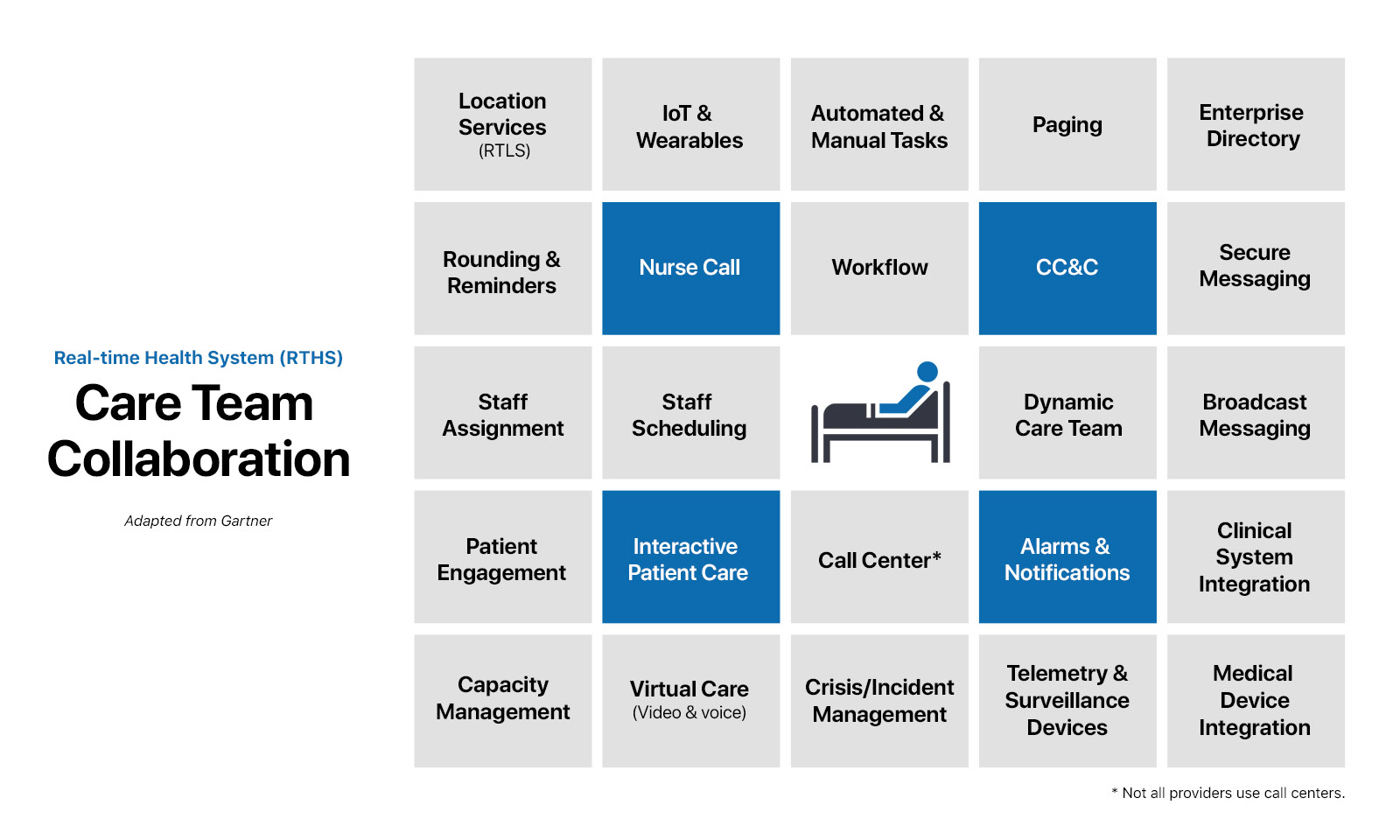
Fortunately, the outlook is not so bleak. A few years back, Gartner set forth a vision for a Real Time Health System (RTHS) that comes closest to defining the future of the digital healthcare industry.
“The RTHS uses information and communications technology to disrupt care delivery as we know it and reduce the time in which medical knowledge is shared, adopted and applied. It uses situational and operational intelligence to determine the need for change or intervention and, in doing so, it eliminates waste and latency, accelerates workflows and business processes, balances resources with demand and improves care quality.” – Gartner
The prerequisite was widespread adoption of EHRs, which united siloed systems. Now, to support value-based, consumer-focused care models, providers seek more situational awareness, care team collaboration, and actionable data for evidence-based decisions at the point of care.
A real-time health system is the culmination of IT technologies spread across all healthcare departments. It’s something a provider assembles with shrewd vendor selections, evaluating each product’s potential to fit their workflows and processes. Real-time health is a continuum, with theoretical perfection at one end, and reality falling somewhere along the trajectory.
An RTHS considers a patient’s total experience with the provider, including before, after, and outside the framework of traditional, brick-and-mortar visits. It addresses all of a patient’s care touch points: their health plan, inpatient and outpatient visits, experiential way finding within buildings, virtual and remote visits, home-based portals, check-in, billing, post surgical surveillance, home care. (RTHS considers even more than these, but we’ll confine this discussion to locations where traditional nurse call is deployed.)
Care team collaboration: a roadmap for nurse call vendors
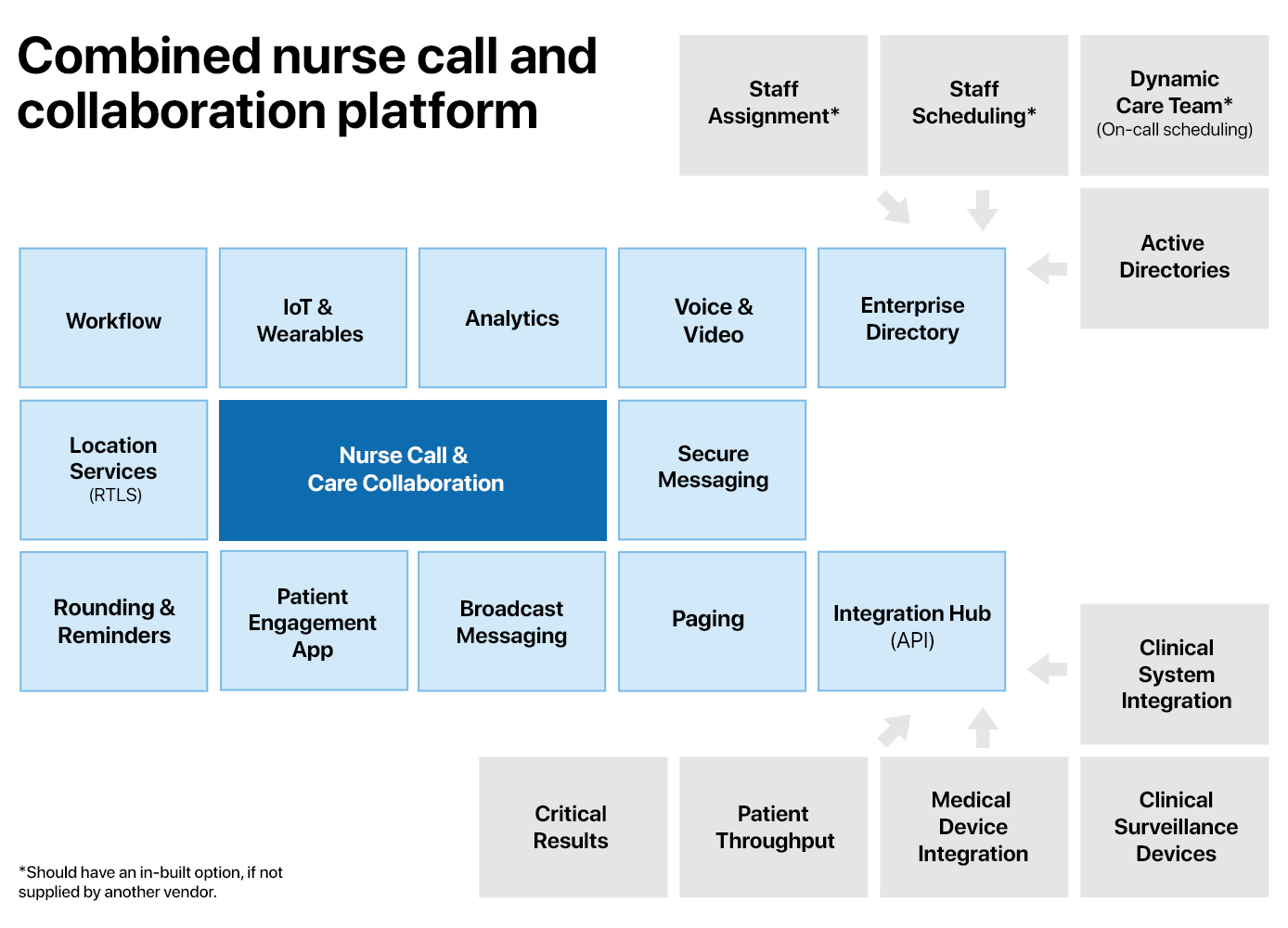
No single vendor has all the components of a real-time health system; nurse call is a piece of a much larger puzzle. The component that includes traditional nurse call, as well as adjacent systems and processes, is called care team collaboration. Software-driven nurse call platforms are positioned to form the foundation of care team collaboration.
There’s been M&A activity around care team collaboration recently, with Hill-Rom’s acquisition of Voalte in 2019, and the software platform TigerConnect acquiring nurse call vendor Critical Alert in 2021. Both point to the critical need for traditional nurse call to find a place in the new healthcare paradigm, which is increasingly software-driven, mobile, and cross-platform.
The following areas, all components of care team collaboration, involve nurse call to some degree. Nurse call vendors need to consider which features they might offer, and how deeply they are incorporated. Make no mistake: providers expect all this and more. Whether home-grown or integrated, nurse call vendors need to have solutions that cover all these areas. All bear consideration in any modernized nurse call roadmap.
Data aggregation with RTLS and IoT
The first requirement for real-time health is real-time data. With that in mind, a nurse call system’s primary function becomes data gathering. Put more accurately, it collects information that enhances the situational awareness surrounding a patient. (“Patient” also encompasses residents in aged care, and independent seniors in their homes and longterm communities.) It records patient behaviors and care-team interactions, enabling staff workflows while contributing to a holistic view of the patient, alongside data from other systems.
Nurse call is symbiotic with real-time location, and both are essential for real-time health. For purposes of an RTHS, nurse call and real-time location are halves of one system. Together, they cast as large a net as possible around patient and staff behaviors. Not just for location sensing – the who, where, and when – but also condition sensing: the state of an asset. If a person, are they upright or prone? How long have they been in a location? How has their activity changed over time? If a piece of equipment, what is its battery level? Is it currently in use, in-stock or expired? If an environment sensor, is the space occupied or empty? What is the ambient noise level or temperature?
Even in markets where providers are not able to assemble a complex real-time health system, location sensing is still desirable for the data it provides to analytics and evidence of care requirements. RTLS systems’ cost puts them out of reach for large segments of the market. In recent years, however, some nurse call vendors have addressed this need by incorporating RTLS functionality directly within the nurse call system, instead of an integration with a 3rd party.
Real-time health is also the internet of healthcare things: wearables for staff and patients, disposable vitals monitors, consumer products that interact with a patient’s smart phone, step tracking, smart beacons, environmental monitors, pill dispensers, and any device that gathers data about patients, staff, and the environment around the patient. IoT devices fill gaps in the data, and provide metrics that previously were not considered part of a medical setting. A modernized nurse call system will likely include an IoT aggregation platform, and certain types of IoT devices naturally fit into a nurse call ecosystem. The platform is crucial because it allows a provider to purchase and use off-the-shelf devices. (Thankfully, there is some movement in updating the UL spec and other regulatory documents to accommodate new products that are not technically part of the system.)
This expanded notion of nurse call is no longer just an on-demand system, whose usefulness begins and ends with the pressing of buttons. Modernized nurse call is always sensing, collecting, and transforming activity and event data, and publishing this information for all systems to use.
It’s critical to prioritize the data’s accuracy, and the speed with which it’s shared, as it forms the basis for everything that happens upstream. Behavioral analysis feeds care delivery for a specific patient, and in aggregate contributes to population health metrics.
Thus, the first step in the modernized nurse call roadmap is embracing its focus as a data capture system, and incorporating real-time location sensing, and other device inputs as part of the system. The “product” is no longer physical buttons and lights. A modern nurse call system sells operational intelligence solutions.
For some vendors, this may be the end goal. How much of a footprint we have beyond that depends on our willingness to embrace new concepts of what “nurse call” can be.
Clinical communication and collaboration systems
Of all the technologies that may displace traditional nurse call, clinical communication and collaboration (CC&C) systems are the most likely. While nurse call vendors start with hardware and build software on top, software vendors have been assuming the functions of traditional nurse call unburdened by the need to connect to legacy hardware. The result is that they’ve addressed the advanced communications side of nurse call more thoroughly than nurse call vendors.
CC&C is the sharing of data about a patient, with information from the EMR, telemetry equipment, beds, nurse call, and other operational systems. It coordinates the activities of the care team around the patient. It broadens the “care team” to include pharmacists, assistants, mental health workers, home health aides, and even patients’ family members. The platforms also attempt to optimize care transitions: physical location changes, departmental handoffs, shift notes, admit/discharge.
CC&C is often synonymous with middleware, and some nurse call vendors have built their own platforms as well. Armed with open APIs and straightforward methods of integration, nurse call vendors can and should absorb the areas now claimed by CC&C. Even more than the hardware, this is the heart of nurse call: moving information to the correct person at the correct time to enable care delivery.
CC&C capabilities include:
-
- Alarm management is something many platforms offer, at least partially because traditional nurse call has failed to innovate. A CC&C platform should be able to take in alarms and alerts from beds, telemetry equipment, predictive analytics software, EMRs, and early warning scoring systems. It should be able to escalate, forward, and prioritize the alarms. And it should be able to send those alarms anywhere the provider requires. Note: alarms and notifications is sometimes a standalone feature, however most CC&C platforms include it alongside communications.
- Messaging. Messaging is built into the core of a CC&C platform. It allows any message, from any integrated system, to be sent to any device or any other system. This applies to automated and user-initiated messages. There is no reason a facility should need another software platform to accomplish this, efficiently and securely. Also includes the sharing of lab results and images.
- Voice calling. VOIP endpoints and integration with existing telephony systems. Most users of voice communication will be on a smartphone over wifi. Needs to negotiate VOIP and real phone extensions, inside and outside the LAN and WAN.
- Enterprise directory. CC&C platforms allow providers to keep a master list of all users within the system. Each contact is assigned to one or more groups and given an appropriate role, so users can call, text, schedule and assign as necessary. The directory needs to allow for multiple sources and Active Directories, staffing, scheduling, and on-call systems. It’s also critical to group users into teams, with dynamic updates, so “crash team” always resolves to the correct contacts.
- Workflow and rounding. Middleware providers recognized that system integration would be the challenge defining advanced healthcare communications. Workflow and rounding make use of all integrated systems: ADT and bed management, nurse call, scheduling, transport, EMRs, labs and medical imaging, any number of other ancillary systems. Workflow commonly includes handoff and shift notes, documentation, and some kind of explicit transfer of responsibility from outgoing to incoming staff. Rounding is typically augmented with risk analysis, so rounding times are calculated based on condition and acuity. Workflow often functions alongside capacity management to minimize bottlenecks in patient throughput, especially around discharge, where delays can cause problems to cascade.
- Analytics and Reports. Most platforms offer built-in metrics for staff and enterprise reporting. This is a must-have, and should include actions taken within the CC&C system itself, including a history of messages sent, phone calls completed, and events that have been pushed to the patient’s EMR. A good vendor will also offer the option to stream the data to the provider’s database for use with 3rd-party analytics, recognizing the practical limits of “doing it all”.
- Barcode scanning. Some vendors, particularly those who make phones, offer integrated barcode readers. Frankly, smartphone cameras have progressed far enough that this is unnecessary – PPIDs, medications, QR codes can all be read by using the camera within a native app.
- Pager support. If not fully replaced with equivalent functionality in smart phone and wearable apps, CC&C must offer integration with traditional pagers.
- Native apps for phone, tablets, wearables.
- Desktop app, or access through web portal.
If there is one flaw in the CC&C vendors’ plans, it is the assumption that every necessary system will be accessible, its data in the correct format, ready to be used. While this may be the case with large acute-care systems in markets where spending is no barrier, there’s a large segment of the market that just isn’t there yet. Particularly for staff assignments, roles, and workflow, a provider may look to the nurse call or other platform to supply these pieces.
The point where a physical button press becomes a digital message is messy, and nurse call vendors have been grappling with it since IP technology was introduced. There is no standard message format – most use some kind of xml – and the effort involved to capture and transform the data is expensive in terms of R&D time and skillset. CC&C vendors have been able to ignore this mess, arriving on the scene once the heavy lifting is done, to offer their advanced features.
Like RTLS, CC&C platforms are pricey, and in some markets they’re out of reach for average providers. In that situation, a nurse call vendor who has built their own CC&C platform has the advantage. Similarly, standalone CC&C has focused on communications, and less on nurse call functionality. The other key advantage for nurse call vendors who have their own platform is the control of the nurse call system remotely through an app. In other words, full system functionality untethered to a physical button press.
The second step in modernized nurse call is to add communication and collaboration features on top of robust data gathering.
Interactive Patient Care
Interactive patient care (IPC) platforms typically offer inpatients some combination of entertainment, access to facility services, research and education, and communication. The platforms are delivered either through an interactive TV, a bedside touchscreen device, or increasingly common, an app the patient downloads to a personal mobile device.
Nurse call’s opportunity is to address the communications component. Specific patient requests can be registered through an app, along with a pain level indicator. A patient app acts as an in-room whiteboard, with information about the current care team members and the means to contact them, the patient’s daily schedule, and a forum for family members to ask questions that care team members can answer through the app. One of nursing’s biggest time wasters is fielding the same questions from multiple family members at different times. Engaging the family through an app offers measurable savings.
Another step in modernized nurse call would be to incorporate some kind of patient app to augment interactive care and engagement.
Patient Flow and Capacity Management
A patient flow solution can address bottlenecks, capacity issues and throughput. A fully-realized RTHS benefits from the sharing of this data throughout all integrated systems. Its relation to nurse call is tangential, but there are a few specific places where such an integration is important.
If workflows exist within nurse call, the results of those button presses need to be shared externally. For example, if nurse call has a “room ready” button for staff to press when a patient is discharged, the patient flow system needs to know when that button is pressed, and environmental services needs to know to clean the room. This is why nurse call vendors must offer an API, not simply a TAP or ASM integration, to share events system-wide.
If ED decides to admit a patient, that workflow action should check with bed management for available beds. Go a step further and assign the patient to a room, which updates the EMR, which updates nurse call. A step further still, use integration with building management to set the environment in the room – lights, temperature, blinds – before the patient is ever moved. If assignments are done by location, notify the staff assigned to the room that a new patient is inbound. These steps may comprise four or more disparate systems, but the communication between them must be as performant as possible.
Besides workflow itself, nurse call’s opportunity is the accessibility of the combined data. Many vendors offer a census board or whiteboard with customizable data points, including ADT, EMR, and other systems’ data. Whiteboards are an opportunity because nurse call stands at the nexus of care and administration. Providers need to determine if the vendors, whose data they want to display, make that data available to other systems. It would be inefficient to have a whiteboard for every clinical system, all with a slightly different data set.
Another step in modernized nurse call, then, is the display of census data and patient statuses, with information coming from patient throughput and other bed management systems, as well as patient data from the EMR. The combined data needs to be portable enough to be displayed on any screen, not only proprietary “nurse call” displays.
Summary
There’s a lot of overlap among vendors and their offerings. RTLS companies make nurse call and ADT-like features. Middleware does the same, plus messaging, even staff management. Workflow and rounding are part of some EMR platforms. There are any number of standalone apps that address messaging and voice communication. All vendors offer some sort of analytics package.
It’s all very messy for a provider, who may need a dozen vendors just to implement their desired solution. The providers rightly question why a piece of data collected at point ‘A’ cannot be sent to system ‘B’, updated, and finally moved into database ‘C’. The truth is this: healthcare platforms can be this tightly integrated. The reasons they’re not have more to do with data silos and turf wars than any technical barrier.
API: the lingua franca of system integration
Conceptually, real-time health is a pub/sub system. Short for publish/subscribe, pub/sub is a IT concept referring to event-driven architectures, where systems communicate with one another asynchronously. To do so, they need a common language and a clear path to register, authenticate and exchange data in real time.
Instead of proprietary integrations, the differentiator will be whether a given vendor has a robust API. In selecting vendors, rather than ask “which systems do you integrate with?”, providers should verify that the vendor can publish events in a continuous, real-time feed. One which other systems can use, as necessary. Vendors should also be able to input events and data from other systems using a standards-based, open source framework, like REST.
Technical skill sets need updating too
Particularly as more data is moved to the cloud, the strength of the network will be paramount. This is an IT puzzle to solve, and many are making strides. In some cases, however, providers may look to their vendors to manage network usage, in which case a nurse call vendor’s core competency, and that of its distributors, needs to include advanced network administration. Ditto cyber security.
To make deployment and maintenance simpler, we nurse call vendors ought to investigate the use of containerized platforms and other means to abstract our software from the hardware that runs it. The responsibility for dependency management and version control falls to the vendor and makes life that much easier for provider IT teams. Load-balancing clusters will become necessary as more providers expect enterprise deployments comprising many buildings and campuses spread across a wide geographic area.
Next: new markets, new products
In the long term, real-time health is only a step towards ahead-of-time health. Predictive applications that prompt behaviour changes to keep people healthy, instead of reacting once they get sick. Precision medicine solutions, and adaptive virtual personalised platforms are in their infancy, and will be enabled with the exchange of real time data. (Critical to the transition, though outside the scope of this discussion, is evolving the fee-for-service model that keeps the focus on treating the already sick, rather than on incentivising prevention.)
For nurse call, the ultimate goal is predictive: alerting caregivers before patients know they need help, identifying developing problems before they become emergencies. The fundamental process underlying nurse call is this: when someone needs help, we provide the means to obtain it. With modernized nurse call, and its emphasis on data gathering and broader communication, we expand that notion to this: based on the data, we think you may need help soon, and will proactively obtain it for you.
In part 2 of this discussion, we will look at emerging markets and product opportunities for nurse call vendors, in light of the broader scope of real-time health. These include AI-backed applications, home care, and voice-controlled systems.