The Facility
William Osler Health System’s Brampton Civic Hospital is an open, accessible, public hospital which provides the community with a modern facility, advanced medical equipment and a comp equipment and a comprehensive range of health services. In addition to paving the way for advanced health care, Brampton Civic Hospital is the largest health care infrastructure project completed in Canada and is one of the first green-field hospitals built this century.

This cutting-edge facility offers increased capacity, providing improved access to safe and high quality health services for the community’s growing population. Patients are more comfortable, with larger, more attractive rooms that are spacious enough to accommodate family members. The massive 1.2 million sq. ft. facility is located in Brampton, Ontario, just west of Toronto and was built to accommodate 608 beds and 18 operating rooms and is the centre of innovation, electronic health records and ultramodern technology.
Challenges
Brampton Civic Hospital replaced an outdated hospital built in 1923 and was designed with the goal of improving the quality, safety, speed and accountability of care to meet standards recently set by the Province of Ontario.
Anna Morgado, Clinical Informatics Analyst at Brampton Civic was involved with implementation and training of the newly installed Austco Nurse Call system and symbol device integration prior to the hospital’s grand opening. At the old hospital, Anna had worked with another nurse call system which she described described as “a box and a bell”. She shares a story from the old hospital of an event where a “ghost bell” was activated and none of the nurses could locate the origin of the call. Through process of elimination, staff went room-to-room pulling out call cords before finally locating the mystery call bell.
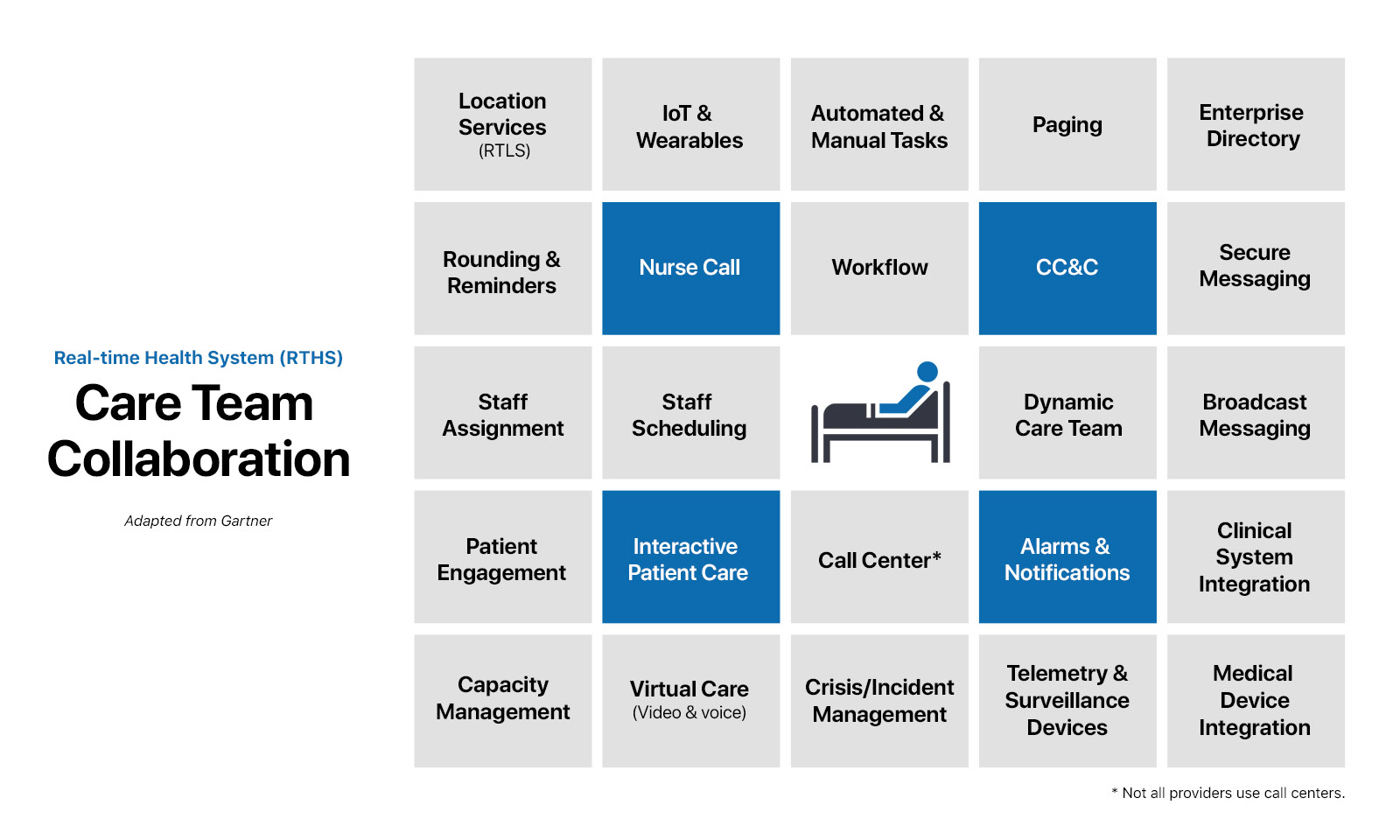
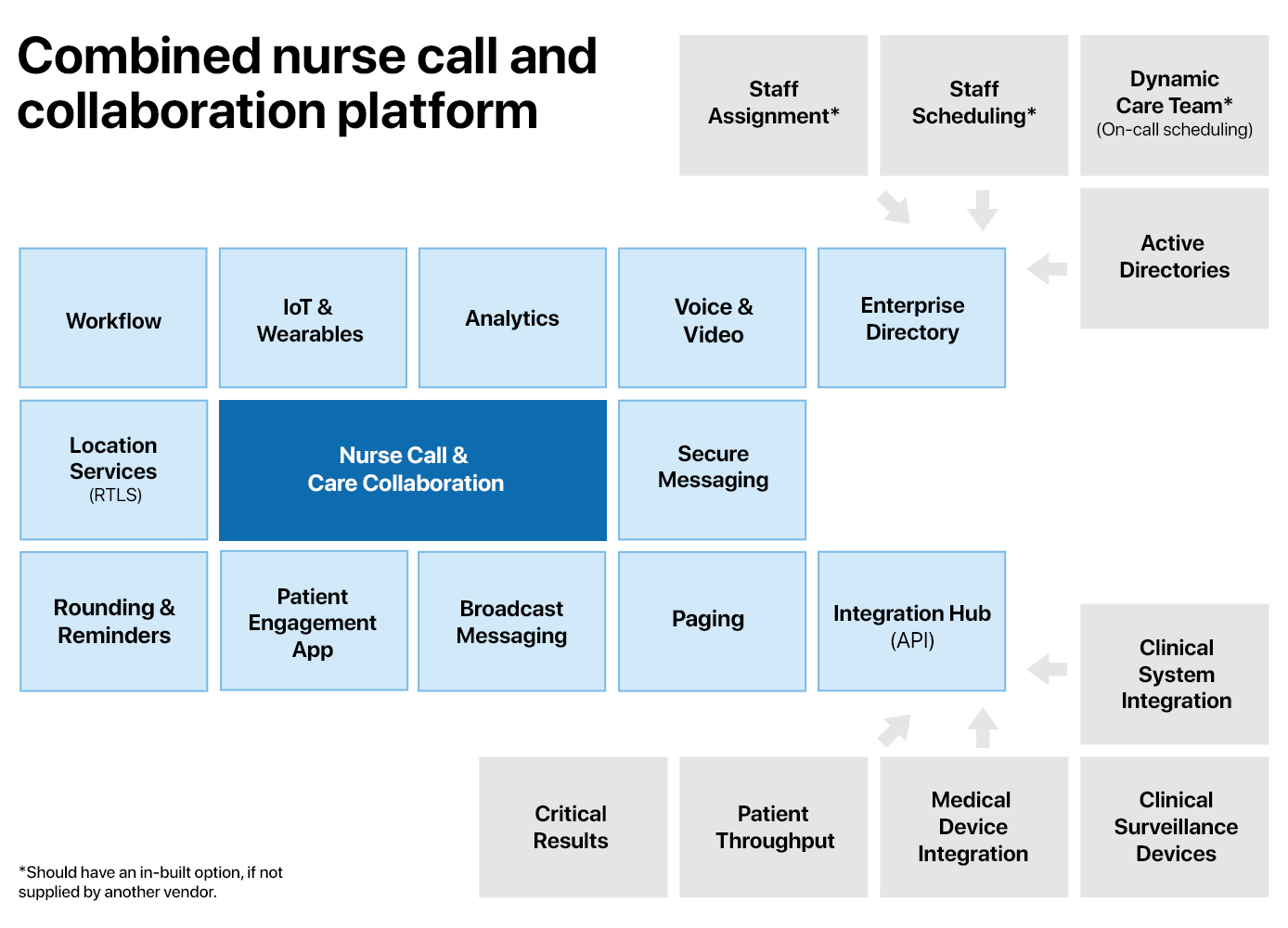
The new hospital needed a reliable nurse call system that would allow staff the ability to provide the highest quality of patient care with optimal responsiveness to patient needs, enhance staff efficiency and mobility plus, reduce intrusive overhead paging creating a quieter environment. The solution would need toto provide an efficient way of answering call bells.
Solution
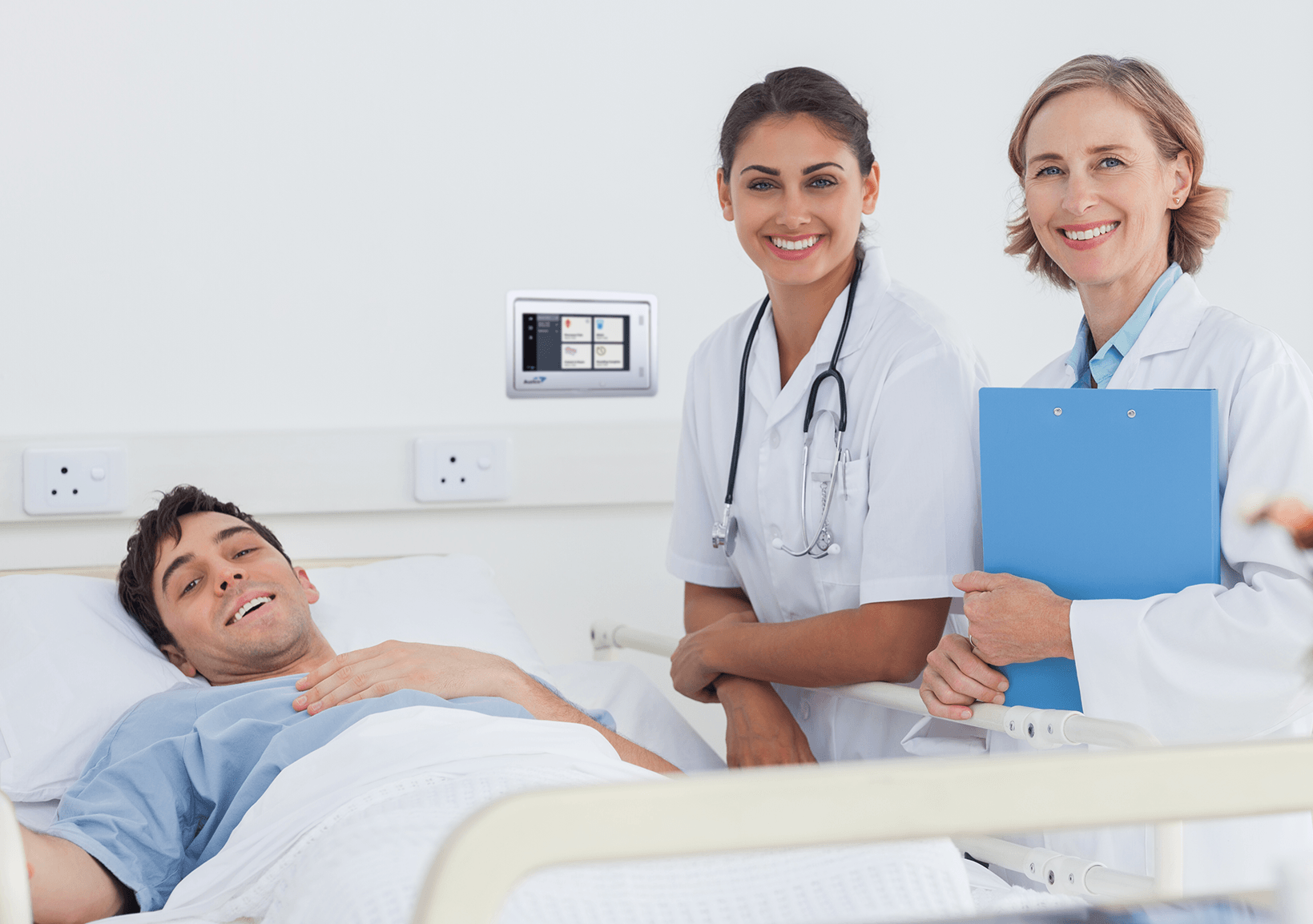
Brampton Civic Hospital implemented an IP Nurse Call System from Austco for its operational flexibility and reliability. The hospital contains over 2800 Call Points (washroom pull cords and patient push buttons), 1600 over-door lights and 50 master stations stations supplied by Austco as well as 500 of Austco’s multi-function pillow speakers for nurse call, TV/Radio and light control.
Outcome
The nurse call system incorporates a comprehensive range of call types and priority levels while the integrated software solution is the glue that streamlines and enhances the communication efficiencies with the nurse call system. This event notification, escalation and reporting application provides the hospital’s management management teams with detailed reports on staff response times, number of escalated calls and call frequency. These simple-to-use reports are generated as needed and provide valuable data to support patient safety and satisfaction.
In some of the units at Brampton Civic, patient requests are routed directly to a designated nurse’s wireless device where he/she is able to communicate with the patient immediately. For calls of a non-urgent nature, the nurse can acknowledge the call in real-time and can either pick up a requested item along the way, or simply answer a question without visiting the room at all. The result is an increase in patient satisfaction, an increase in nurse productivity and staff members no longer need to send noisy overhead pages to locate a nurse which creates a more quiet and healing environment.
All News and Events