Smart watches & wearables
Wearables clearly have potential in healthcare. It’s been unrealised potential though, as only the most advanced watches can run anything more than a step tracker. Only recently have they come down in price to the point a facility could consider providing them for staff. And until recently, all such devices needed to be tethered to a phone.
For staff
A smart watch offers alarm and notification management hands-free; smart watches are ideal for managing incoming notifications. As battery life improves, allowing for voice communication and processor-intensive apps running for the duration of a 10-hour shift, the watch may well be the only piece of communications equipment staff need carry. Along with a bluetooth earpiece and controlled by a voice assistant, most of the functions of care team collaboration can be completed with a smart watch.
The data generated by the watches contributes to bottom-line metrics. Staff time spent bedside and response times, combined with other patient metrics like call history and acuity, allow a provider to calculate the cost of a patient’s care in real time. (I am aware how dystopian it sounds to picture a changing dollar value next to each patient, like a malign stock ticker. But we’d be kidding ourselves to think that doesn’t happen already.)
And at their core, wearables are gathering data about movement, rudimentary telemetry, so staff are able to chart their own workload over time. With RTLS or GPS abilities, watches become tracking and mobile duress devices.
For Patients
There are (non-watch) wearable devices that automatically report ECGs, HRV, temperature, and blood oxygen levels. Smart bandages that monitor wounds and automatically administer drugs in response to PH and temperature changes. Smart hearing aids, masks and activity/motion sensors. Watches that can read blood pressure. All should be considered as inputs to the data-gathering nurse call system, integrated as part of a robust IoT platform.
For nurse call vendors, the question for wearables is integrate, build, or buy. Such devices are different enough from our core competency that integration seems the likeliest route. The function of a wearable like VitalConnect’s Vital Patch, for example, is complementary to nurse call, and augments data gathering for the foundational layer of real-time health. On the other hand, a smart watch version of a care team collaboration app for staff, and an emergency alert for patients and residents, seems to fit nicely with nurse call’s core purpose and might be built in-house.
A smart watch is an ideal alerting mechanism for patients and especially long-term residents. If they’ve fallen, or otherwise need assistance outside their room, the watches, backed by geo-positioning, can send alerts and exact locations. This is on top of their in-built health monitors. Smart watches dovetail nicely with the limits of RTLS monitoring. Once there are no more sensors, an RTLS system effectively “loses” you. That means any open outdoor spaces either need sensor equipment or some kind of alternative locating, such as a watch’s GPS.
There are any number of companies offering wearable medical alert devices. A lack of regulation means there are a lot of low-end solutions. These are standalone systems, have their own software platforms, and all are built to connect the wearer with emergency services. While that is a fine business model, the opportunity for a nurse call vendor is to take this concept, create a smart watch app, and connect it to a monitoring service – essentially a cloud-based nurse call system. It functions either as an extension of a home care platform, or in combination with a facility’s nurse call system, or entirely standalone. In any scenario, the data is as much a product as the hardware and software, and contributes to a real-time health ecosystem.
An emergency monitoring system, backed by wearable alert devices, gives longterm care a way to reach clients who are pre-need. The value proposition is essentially, “we know you aren’t ready to move into one of our communities yet, but we can begin looking after your health while you’re still in your own home.” Data collected outside the boundaries of a healthcare setting becomes useful once a resident does enter a facility. The more data, the better to show trends and progression.
Obviously the integration of wearables depends on a vendor’s roadmap. If your strategy is to own everything in an acute care room, Hill-rom’s recent acquisition of BardyDX makes perfect sense. If a vendor can summarise its strategy as “get medical help, anywhere”, or has in its client base many longterm care communities, then perhaps a medical alert system complements its product portfolio.
Voice Control and Voice Assist
Voice assistant devices are a natural fit for nurse call. Smart speakers and voice controlled devices like Google Home Mini, Amazon’s Echo Dot, and Apple’s HomePod Mini tick multiple strategic boxes: data gathering and efficient communication.
Nurse call has the opportunity to build in voice control at a fundamental level. Not just a means to signal a call (effectively a high-tech button), they also give us expanded communications and engagement options. Of course, they’re also a means to signal a call, but “hey Siri, get a nurse” is only the most obvious use.
There are companies who have built robust products around voice commands in healthcare. There are user accounts, data synced with EMRs, administration of each resident’s available voice commands, all the required mapping to translate “call Lisa” into the appropriate family member’s phone number. Even which cable news network to show when they say “turn on the news”. Importantly for HIPAA and other regulatory standards, the platforms provide the means to remove any identifying data before the information is sent outside the building.
Further uses include reassurance that help is on the way, once confirmation returns from the Alexa/Google/Siri server. A smart speaker is another VOIP endpoint, capable of making and receiving calls. It can be another input element for residents and patients to control room functions: lights, blinds, HVAC, television. In a common area, it’s another annunciator.
Longterm care facilities already use smart speakers for resident interaction, streaming music and TV. They particularly like the ability for residents to ask questions and receive answers, freeing up staff resources. Residents can ask “what’s for dinner?” or “what’s on the schedule today?”, and it queries an internal database.
This is a technology that builds atop others. For example, residents can use a voice acknowledgement for a morning check-in, instead of pressing a button on a pendant. In combination with RTLS, it becomes possible for staff to ask the system “where is resident Janice?” and the system queries the location database and provides a response. Further, use the speakers to connect a call from wherever the staff member is to wherever resident Janice is. It becomes a mobile duress trigger, as the speakers are fixed points with mappable locations. Simply saying “get help” in a location with a speaker triggers a staff assist or similar.
All interactions with the system can be logged for reporting, and they become further data points in a holistic resident view: is he/she completing more or fewer calls over time? Are they using it to achieve fewer goals? Calling fewer people? All point to a change in condition.
Voice control gets audio into more facilities that might not otherwise pay for it, and could function as a kind of entry-level nurse call system in non-regulated environments. COVID has raised interest in audio, and other hands-free communication options. Home hubs like Google Nest Hub, Facebook Portal and Amazon’s Echo Show also add video calling to the mix. Video calling is an increasingly common remote care method, forming part of care team collaboration and interactive patient care. (As an aside, it would have been a visionary move for nurse call vendors to get into the Telehealth market during its infancy, as it is philosophically similar in its goals and functions. We ought to be investigating AR and VR applications, to enable things like virtual rounding in the future.)
This is a fledgling market, and there are several innovative companies who’d make great partners (or acquisition targets) for nurse call vendors. This is an area where there’s advantage in acquisition, as there are unique challenges around multiple device management that nurse call has already addressed. Additionally, platform makers are careful not to claim their products constitute a life safety system. Nurse call vendors know how to incorporate such devices and their proper classification within regulatory standards.
Home care: off-the-shelf IoT devices + software platform
Some government models reimburse healthcare organisations if they can provide care while letting people remain in their own homes. Combine that with any number of average consumers who’d like to have peace of mind that their ageing parents and relatives are safe at home, and you have a ready supply of customers for remote medical monitoring. The home care market has exploded in certain regions, and looks to be growing everywhere. There are a lot of startups in the space, as the regulatory obligations are less burdensome.
Right now, one can go to an electronics store and purchase bluetooth-enabled pill dispensers, motion sensors, smart pillows, smart locks, electric outlets, lights, cameras, even smart night lights. All of these devices’ data, when taken as a whole, can monitor the health and safety of someone inside a home or apartment. The catch is that they all have their own app and service platforms, and none are fully integrated with healthcare monitoring in mind.
One area of expansion for a nurse call vendor is to combine these off-the-shelf devices with a custom software platform that takes in the data, learns routines and normal patterns, and takes some action when there is a break in the pattern. The product is a subscription service, comprising a software data platform, and apps for family and medical personnel to monitor.
Along with wearable alerting, a longterm care provider can extend its reach into the community, installing a home care system as a way to secure future residents. Such a model is also an advantage over the standalone startups in the field – when deployed as part of a longterm care community, the service is backed by the heft of an existing nurse call system and a ready team of medical personnel. In addition to the system itself, we also have the data it generates feeding individual resident’s health records, and taken as a whole, population health metrics.
Large tech companies have offered this feature and its attendant apps, trading on their supply chain to keep costs down on the hardware side. Some standalone companies in this space, lacking the full array of sensors and smart devices, instead use low-end nurse call hardware, like pendants and pull cords, and their service stops at the point of connecting a person to a care provider. In both cases, they are isolated systems.
Taken a step further, longterm care corporates have begun outsourcing off-hours help to companies who coordinate independent nurse visits to homes and apartments. A logical extension of the platform would be an automated medical dispatch service. At the risk of a trite analogy: Uber for nurses, automatically assigned, based on monitor data, and resident data shared as part of a real-time health system.
Clearly, home care is an adjacent market, and B2C may not make sense for every vendor. However, “nurse call for all” has a certain marketing ring and quite a bit of potential in the new world of COVID isolation and seniors’ desire to remain in their homes as long as possible.
Machine learning
If there were a critical, yet still unrealised, component of real-time health, it would be the machine learning engine. Machine Learning (ML) is a friendlier term than AI, and more accurately reflects that the core function is to examine – or “learn” – massive sets of data to recognise patterns, in order to take action when it detects a change in the pattern.
Real-time health does not depend on a single, all-powerful engine. Instead, there can be multiple ML applications, each optimising a different part of the system. To get maximum functionality across all their vendors, providers themselves need to take the lead in deploying their own decision engine. One based on their processes, crunching their data, and answerable to their leadership team.
Instead of trying to control the entire continuum, we individual vendors can apply machine learning internally. Nurse call vendors can optimise and amplify the things that nurse call already does well: using technology to get help, and streamlining the flow of communications. To properly train an ML engine requires enormous amounts of data, and we can only guarantee access to the data we produce. We have alarm and call histories, RTLS location data, communications history, and patient/resident activity history. Given access to some EMR and other real-time data, we can offer predictions and analysis in a few ways.
Predictive Alerting
Traditional nurse call gets medical help when you need it. Modern nurse call, informed by machine learning, gets medical help before you know you need it. Modern nurse call is intelligent nurse call.
As stated, the goal for nurse call is predictive: alerting staff before patients know they need help, identifying developing problems before they become emergencies. Predictive alerting is the ultimate evolution for nurse call. It takes the spirit of the system’s core purpose and moves it into a future where the entire care environment is constantly evaluating data, looking for anomalies, ready to take action.
As an example, consider an automated message delivered to a nurse’s smartphone: “check on room 10”. In response to the patient sitting up in bed, the nurse call machine learning engine, let’s call it “Florence”, has examined the patient’s call information and activity over their stay, and the amount of time care team members have spent in room. Florence has checked the patient’s telemetry data over the last few hours, compared their vitals and lab results against patients with similar diagnoses, and based on the total data, calculated a 47% chance of developing a complication. With that percentage, the rules set by the facility specify a wellness check (as opposed to generating an emergency alarm), and therefore Florence has directed the patient’s nurse to check in. Had Florence predicted something serious – a higher probability of complications, sepsis, or an immediate life-threatening event – the intervention would be suitably more urgent.
Instead of a button press as the catalyst for action, intelligent nurse call evaluates each new piece of data from any connected system for possible red flags, and automates the response. Particularly for button presses in extremis, intelligent nurse call should have already noted a decline and alerted someone before the patient picked up their handset, before staff arrived to find the situation deteriorating into emergency.
Broadly, the move to predictive alerting mirrors the conceptual transition healthcare needs: fee for service is oriented towards the already sick, while population health purports to nudge people towards better everyday behavior before they’re sick enough to seek treatment. Similarly, a frantic push of a nurse call button is already too late, in a sense, to address the issues that intelligent nurse call might have seen developing.
Call Routing and Rounding
With the knowledge of a patient’s call history, combined with care team locations from RTLS, Florence can route calls to the nearest staff member, or the nearest staff member with a certain role. The future might be to combine this with patient telemetry information, such that Florence knows which staff members have the best bedside manner while assisting this patient, based on a reduced heart rate or blood pressure.
Rounding as a whole may be automated. Florence can consider the acuity, call history, medication and its potential side effects, current and recent telemetry for each patient. Since it knows staff members’ physical location within a unit or ward, it can take into account distances and routes, and generate a prioritised rounding checklist. With RTLS, rounding is recorded when the staff member walks into the room, and a message recorded in the patient’s health record.
If a care team member receives a high-priority call before rounding is completed, Florence can recalculate and assign other nearby staff the rounding tasks.
Staffing Recommendations
Florence can make staffing predictions based on patient acuity and care requirements. For example, is there equipment in the room, or tricky procedures to perform requiring someone with certain role or experience level?
It considers both patient/resident requirements, and also staff strengths. Quite literally strength, if the patient – a heavy male – needs help getting up from bed. Based on facility standards, the ML-informed staffing can auto assign staff for proper coverage, and the charge nurse has only to verify the decisions.
Behavior Monitoring
Applied to longterm and dementia care, where a long history of data exists, Florence can alert staff if the resident is spending more time motionless, if their nighttime bathroom habits have changed, if they have a decrease in activity as reported by their RTLS badge. Are they using their voice control to complete fewer tasks? This data all points to the condition of the resident, and thus their level of care required. In some markets, evidence of care requirements is the most important piece of data in submitting a claim for reimbursement.
All this data exists today, but still requires a human to review and draw the proper conclusions. Machine learning’s strength is repetitive data crunching, and in that regard it performs more accurately and more efficiently than a person.
Summary: machine learning is promising but still theoretical
If machine learning is the single most important component to real-time health, its development is also the most challenging. There are non-technical reasons for this. Access to enough representative data is one, and as we learned pursuing interoperability, the keepers of the data may not want to share. Additionally, there is no data science competency model upon which to base ML decision making. Or rather, there are too many: one for every decision a healthcare employee makes. Which is the right one to enshrine in the code?
For these reasons alone, it’s necessary to keep the focus narrow. Nurse call’s purpose is to get medical help. It’s not decision support or population health (although our data may feed those systems), nor any of the other areas commonly cited as ripe for ML application. Machine learning in nurse call is an ambitious goal to be sure, but definitely one worth pursuing.
Conclusion
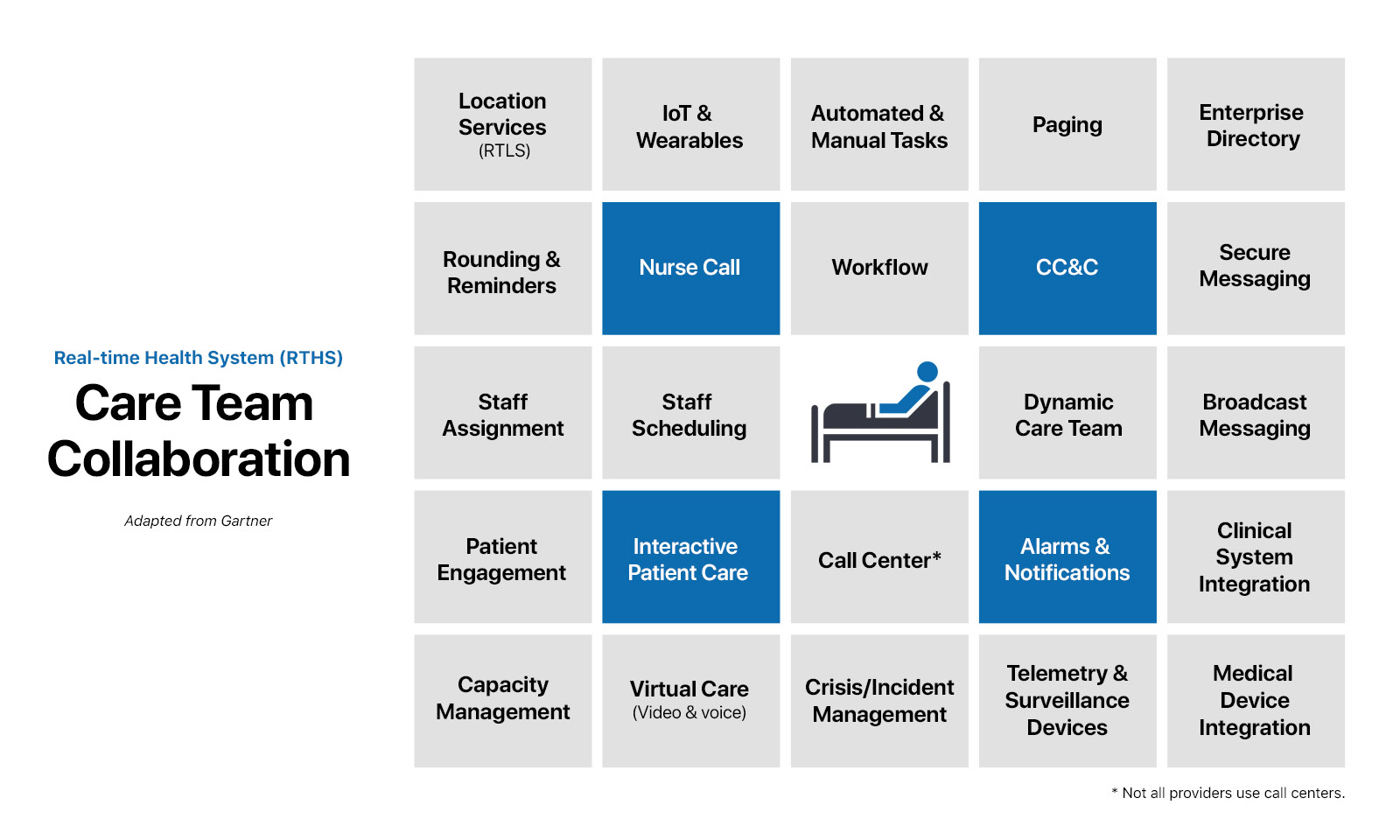
A longterm strategy for nurse call cannot simply be more advanced ways of raising an alarm. We’ll instead need to consider a broader application of our core purpose when evaluating opportunities.
In the book Built to Last, Jim Collins made the point that a company’s mission, clearly stated and internalised by employees, may necessarily pull that company into unexpected markets. If a nurse call vendor’s mission is “to make the best nurse call system”, there is no room for growth. If, however, the core philosophy is closer to “get medical help, when and where you need it”, that company enjoys many more opportunities.
Technology should’t be a barrier between patients and their caregivers. Automating as much functionality as possible frees caregivers from the non-productive tasks imposed by modern healthcare: charting, data collection, remembering to push certain buttons on the way into or out of rooms, tracking down the correct person. Think of intelligent nurse call as a sentinel, ready to intervene if necessary, but receding to the background when not needed.
As stated, traditional nurse call won’t evaporate overnight, but hardware-based alerting within a siloed system will become less relevant to a modern care environment. The future is software, the future is mobile, the future is adaptive. The future is intelligent.